Professor Hoermann responded to statements from Finnish endocrinologist
Professor, MD, PhD, endocrinologist Rudolf Hoermann has retired from the Lüdenscheid university hospital (University of Bonn), where he was head of the departments of general medicine, gastroenterology and endocrinology. He has authored and co-authored more than a hundred articles of reviews in international medical journals. His latest work shows a strong interest in personalised medicine and includes a series of articles on thyroid regulation in peer-reviewed international journals which are among the most read in the field.
Professor Hoermann has kindly commented on some statements from Finnish endocrinologists.
The bold text is Finnish, the normal is by professor Hoermann.
Response to Finnish statements about the care of hypothyroidism
1. Statement by the Finnish Association of Endocrinologists 2014
Free T3 is not needed in diagnosing hypothyroidism.
Free T3 measurement is diagnostically useful and supportive to identify patients with impaired ability to convert T4 into T3.
This is important to monitor because the biochemical response to levothyroxine (LT4) treatment turns out to be quite variable (Midgley et al. 2015). Generally, conversion efficiency is frequently compromised in patients on LT4 treatment, particularly in patients without a thyroid gland after total thyroidectomy, compared to a healthy population or the level of the same person prior to surgery (Gullo et al. 2012, Ito et al. 2012, Hoermann et al. 2014).
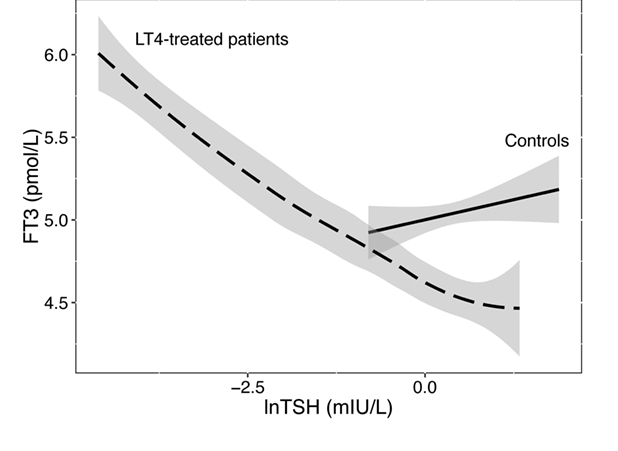
Importantly, TSH and the biologically active FT3 dissociate on LT4 treatment (Midgley et al. 2015, Hoermann et al. 2016). This dramatic change in the equilibria between TSH, FT4 and FT3 has important consequences. Firstly, TSH can no longer serve as a reliable marker of “euthyroidism” then (Hoermann et al. 2013, 2016,2017). In other words, a TSH in the reference range does not guarantee that the patient may be “euthyroid” and everything is well. The reliance on a “healthy TSH range” is a fundamental error in my opinion, not taking into account the altered physiological state that settles and converges on entirely new and different equilibrium than in the previous healthy state (Gullo et al. 2012, Ito et al. 2017, Hoermann et al. 2015, 2016,2017).
This could explain, at least in part, why so many patients remain dissatisfied with the standard LT4 therapy, as has been well documented for instance by assessment of their quality of life. Danish authors have recently conducted a very careful study with a newly developed validated thyroid-specific questionnaire and arrived at the conclusion that patients on LT4 generally fail to recover to the level of the healthy population (Winther et a. 2016).
This means there is definitely a need for improvement in patient care. Measurement of FT3 contributes substantial additional information to monitor the situation where TSH falls short. Other illnesses have to be considered as they may interfere with its interpretation, and a doctor is needed to bring all the information together, not a thyroid test or a lab report.
Reverse T3 (rT3) is of no use. rT3 is an inactive thyroid metabolite, the concentration of which follows the T4 concentration.
Reverse T3 is not an inactive metabolite as has long been thought, rather it acts as a T3 blocker. Our whole view on the non-classical hormones has dramatically changed in recent years and new roles are emerging (Hoermann et al. 2015).
Using the DIO2 gene polymorphism test does not provide information about whether the patient would benefit from T3 (trade names Liothyronin and Thybon) therapy instead of T4 therapy.
There may be an easier way and cost-effective test available, the simple FT3/FT4 ratio. This is generally impaired and low in LT4-treated patients, compared to healthy subjects, and it has symptomatic consequences (Midgley et al. 2015, Winther et al. 2016, Larisch et al. 2018).
Subclinical hypothyroidism should always be treated, if TSH ≥ 10 mU/l. Treatment of less severe subclinical hypothyroidism is warranted by positive TPO antibodies, young age, goiter and hypothyroid symptoms.
Based on thyroid physiology, this statement is incorrect, because the same TSH level can mean vastly different things to different persons (Hoermann et al. 2017). The TSH value cannot be interpreted in isolation (Hoermann et al. 2016, 2017).
The pituitary hormone TSH is required for lifting thyroid hormone concentrations up to their healthy levels. A patient without TSH is hypothyroid, as experienced for instance by patients with secondary hypothyroidism due to pituitary disease.
This creates a dependency and interrelationship between TSH and the thyroid hormones, which are paired. Consequently, a multivariate or paired reference range has to be regarded as more correct than the univariate statistical distribution of TSH by itself (Hoermann et al. 2016). The outcome of such a scenario makes it easily possible that a certain TSH value one patient feels already hypothyroid at may be in the hyperthyroid zone for another patient. This is termed a personal set point or a conditional settling point. The TSH-FT4 pair displays much less variation in a person and a lower individual tolerance and does not match the wide TSH reference range in a population (Hoermann et al. 2017).
Therefore, TSH is a very special and individual controlling parameter that cannot be simply interpreted like any other statistical parameter or laboratory value. TSH is non-normally distributed in the population and tied to FT4 and FT3. The physiologically based set point distribution of the TSH-FT4 pairs in a healthy population is kite-shaped and it looks totally different from the conventional rectangular reference range (Hoermann et al. 2017). An oversimplified TSH interpretation is unjustified by thyroid physiology (Hoermann et al. 2010). It is therefore only helpful as a screening test but not as a reliable diagnostic test.
The T4 maintenance dose is correct when the patient feels well and TSH and free T4 are within the reference range. Generally TSH should be around 1 mU/l.
When “the patient feels well” introduces a notable restriction on the general statement. This invalidates it more often than there is confirmation.
Danish authors of a recent QoL study have the following to say, quoting (Winther et al. 2016) “Many aspects of HRQL improved during the first six months of LT4 therapy, but full recovery was not obtained. Our results may help clinicians inform patients about expected clinical treatment effects.”
The TSH claim has been refuted above.
NDT (trade names Armour Thyroid and Thyroid) should not be used for the treatment of hypothyroidism.
NDT is an approved prescription drug in the USA, so it should be eligible for use by doctors and patients if they so choose. There should be no disqualification of approved drugs. It should be the right of the doctor and patient to choose any drug that is approved by the relevant authorities.
Synthetic triiodothyronine (T3, trade names Liothyronin and Thybon) should not be used as monotherapy for hypothyroidism, because it will easily lead to T3-toxicosis. During therapy TSH should never be less than 0.1 mU/l.
T3 is not a drug of first choice, but it has been used for a long time, particularly after withdrawal of LT4 in preparation for radioiodine therapy. There is a long history of practical experience with T3 in many countries and it remains an approved drug with a good safety record. This warning about T3 toxicity seems appropriate but exaggerated. There are more realistic reports on its use, for instance by Leese et al. (2016).
We have been safely treating thyroid patients over many years in a TSH suppressive manner as required by the previous thyroid carcinoma guidelines. Those requested to keep TSH fully suppressed at all times because of a fear that TSH may stimulate growth of residual cancer cells in the body and promote the relapse of the cancer.
A TSH of 0.1 does not mean the same for a patient on LT4 as it does for a healthy person, as explained above (Hoermann et al. 2017). Hence, this is an unsupported averaged conclusion.
For safety studies, thyrotoxic patients on LT4 and naturally hyperthyroid patients must be viewed separately and viewed differently. Frequent mixed reports have to be dismissed. For classification of thyrotoxicosis, FT3 and FT4 must be considered as well (Hoermann et al. 2017). A low TSH by itself is ambiguous and not sufficiently interpretable, since any interpretation of dissimilar entities is prone to fall victim to a statistical amalgamation bias, also known as the Simpson paradox.
Because the half-life of T3 is short (around 24 hours), the problem with T3 treatment is the huge diurnal variation in T3 concentration.
FT3 has a natural circadian rhythm, as does TSH, but not FT4 (Russel et al. 2008). That means it also naturally varies more than FT4.
The risk of combination treatment is thyrotoxicosis caused by a too large T3 dose. This can be seen as low TSH, even if the free T3 taken before the medication is normal.
The risk must and can be monitored by measuring all three thyroid parameters TSH, FT4 and FT3 (Hoermann et al. 2017, Larisch et al. 2018). That is why FT3 assays are needed. The isolated TSH measurement is inadequate. Of course, symptoms must also be monitored to adjust dose when required.
2. THL/FinOhta literature survey, part 1, 2015 (for Palko)
As a summary to answer question 1 we can conclude, that measurement of serum T3 and rT3 are not reliable in diagnosing hypothyroidism.
The strength of FT3 is to identify a lack of conversion, which is also important to recognise and monitor on LT4-treatment, not so much diagnosing primary hypothyroidism as such. For the latter, TSH is more sensitive, but also less specific.
Can synthetic T3 be used as monotherapy in hypothyroidism?
The publications of Celi et al are the only RCT:s, where T3 monotherapy has been compared with T4 monotherapy.
Apart from the Celi trial, there is ample experience and literature from nuclear medicine specialists where T3 was and still is commonly used for bridging after T4 withdrawal in preparation of radioiodine treatment.
While this addresses the short-term use of T3 very well, there are reports that suggest long-term safety concerns should also not be exaggerated and used for scare mongering (Leese 2016).
3. Palko statement 2015, now deemed unlawful
There is not enough scientific evidence on treating euthyreotic patients for depression or obesity. The available scientific studies have not adequately estimated the safety and tolerability of the treatment.
It is scientifically proven that thyroid hormones are pharmacologically effective as a mild antidepressant. They may well be used for that purpose with the advantage of lower side effects, compared to genuine antidepressant. This applies to mild depressive syndromes only, not to severe psychiatric disease. Again, they do work safely if used correctly and doctors and patient should be able to make that decision. And they should be available to the public and funded as any other approved drug. They are no more dangerous or expensive than antidepressant and they may well be worth a trial in mild cases.
4. Review article in Duodecim magazine 1/2016
TSH is the main follow up parameter for the treatment of primary hypothyroidism. Its concentration should be 1 - 2.5 mU/l in young adults, but it can be higher in middle aged and elderly patients.
The statement is unfounded and contradicted by scientific evidence because the equilibria are different on LT4 from thyroid health (as discussed above). And they are highly variable by person and by disease entity so that the use of an average is misleading for the care of individual patients. Thyroid physiology has been explained above and as for the statistical use, the Simpson paradox has to be considered and avoided whenever clustering applies (Hoermann et al. 2017).
In the 1990s it was found, that normal T3 and T4- concentrations were not achieved in all tissues of thyroidectomised rats on T4 monotherapy. T3 was also required. Because of this, several clinical investigations were started, where T4 treatment and T4 + T3 combination treatment were compared. The studies and their meta analyses didn't, however, show that the combination treatment was better, and the risk of T3 thyrotoxicosis on combination treatment was discovered.
They did not show that T3/T4 combination was ineffective or worse either, and in fact most patients did favour combination when asked about preference at the end of the trials. Why would the patients consistently opt for one over the other in blinded trials? A plausible explanation to consider and further examine would be that it must have had some effect that was not captured by the QoL or the statistical analysis.
There are no RCT studies on the prognosis of the treatment of hypothyroidism.
The prognostic studies vary widely in their reported outcomes, contradict each other and may suffer from group dissimilarities, as discussed and reviewed elsewhere (Hoermann et al. 2017).
In primary hypothyroidism the most important lab test, when assessing the response to T4 treatment, is TSH, which should be within the normal range. In central hypothyroidism, originating in the brain or pituitary gland, the follow up parameter is free T4, which should be at least in the middle of the normal range.
The addition of FT3 and measurement of all three thyroid parameters is required to complete the clinical picture and capture the efficiency of the conversion process, which may vary widely and often dissociate the FT3 response and the TSH response (Hoermann et al. 2013, Midgley et al. 2015, Ito et al. 2017).
A high TSH combined with a free T4 within range indicates bad attitude against the treatment. This happens, if the patient forgets to take several days' medication, and then takes extra T4 doses just before going to the laboratory.
If the patient doesn't feel well, check first that the patient takes the levothyroxine regularly according to the instructions.
The reasons for the patients not feeling well are mostly unclear, but for some patients, explaining factors might be the psychological burden of the thyroid disease, other psychological symptoms, somatisation, other concurrent disease (anaemia, inflammation, hypercalcemia, diabetes, B12 vitamin deficiency), the thyroid autoimmunity itself or other autoimmune disease. These should be assessed as possible causes for the symptoms.
Of course, this all may occasionally happen. But it is an unlikely explanation for the scale of the well documented discrepancy in QoL outcomes, compared to the healthy population.
It is reasonable to check diseases that may be associated with autoimmune thyroiditis, but in general the blame should not be shifted back to the patient for general shortcomings in the treatment strategy.
It has been speculated, that in some patients a lower free T3/free T4 ratio might indicate a lesser T3 conversion in peripheral tissues, which would not be enough to compensate for the lacking T3 production from the thyroid gland. There's no scientific evidence about this, and the T3 production of peripheral tissue can't be measured in clinical work.
If the patient has no thyroid gland where should the T3 come from and why would a low FT3 level not indicate some shortage in the production chain, in perfect agreement with the evidence derived from animal studies (Escobar-Morreale et al. 1995, McAninch et al. 2015, Werneck de Castro et al. 2015). Empirically, it has been well documented that raising the FT3 does help (e.g. Larisch et al. 2018), and many patients can readily attest to this fact.
On LT4 treatment, serum FT3 levels become instable. Auto-regulation that stabilises the FT3 level over a wide TSH range in a healthy person does no longer work in the athyreotic patient (Hoermann et al. 2016). This difference between thyroid health and disease is very important to appreciate. What once was nothing to worry about is a major concern.
Because the real clinical meaning and the correlation of the complaints about remaining symptoms of the free T3 measurement are unclear, we don't at the moment recommend that a general practitioner should use free T3 measurement during T4 therapy. More studies are still needed especially for patients on T4 therapy, whose symptoms linger.
Perhaps, no more studies are needed, but better statistical analysis. Thyroid hormones have a high individuality index, which has been well recognised since the pioneering work of Andersen et al. (2002). But this has not been translated to the statistical trial analysis. As each patient moves on its own trajectory and settles at a slightly different optimum value, simple statistical averaging across groups, such as a treatment and control group, is not applicable and appropriate, it requires the use of more sophisticated techniques such as multilevel models, where a variable outcome at the subject level is accounted for.
With the use of such a model the association of symptom relief with a change in FT3 concentration could readily be demonstrated in a large retrospective study (Larisch et al. 2018). In accordance with the patient experience, reported symptoms were more likely to be present with a low FT3 and to disappear when the FT3 was raised.
Of course, people can be tired for various other reasons as well and this should be investigated as appropriate, but if FT3 is low in an otherwise healthy person, why not rectify that first and see if it helps.
In the clinical work the T4 dose can be fine-tuned according to the symptoms, but the values should remain within the reference ranges.
This tenet has been refuted by a number of carefully conducted studies by our group and Ito et al., as discussed above. We should also keep in mind that just a few years ago the thyroid cancer guidelines requested complete TSH suppression. Every few years the guidelines suggest a dramatic change of actions, and doctors and patients should just follow along on the ride.
Some patients feel well, when the values are close to the border to hyperthyroidism (TSH close to the lower border and free T4 close to the upper border of the range). Some feel better, when the values are close to the border to hypothyroidism (TSH close to the upper border and free T4 close to the lower border of the range). Significantly increasing the T4 dose is not recommended because of adverse effects linked to hyperthyroidism.
Recommendations cannot be averaged, but they must be individualised. Ranges are different in patients on treatment from thyroid health and this translates to measurable differences in outcomes including surrogate markers for tissue T3 effects (Hoermann et al. 2015, Ito et al. 2017).
T3 monotherapy easily leads to T3-thyrotoxicosis (TSH suppressed, free T4 low and Free T3 high). T3 therapy poses a high risk for atrial flimmer and its complications and a risk for osteoporosis and bone fractures.
Doctors have safely known how to deal with T3 for many years, but they have individualised the dose and adjusted it as required. So, it is not the T3 that appears to be at fault here, rather the guidelines attempting to average all patients. This may lead to undesirable outcomes, as might be expected in a highly individual parameter. As the high individuality index of thyroid hormones has been clearly recognised and acknowledged, it should equally be considered and applied to the treatment situation.
The treatment of choice is synthetic human levothyroxine. The goals for treatment are amelioration of symptoms and normalization of TSH and free T4 concentrations.
This is true, but it describes an unlikely combination that animal studies found not to coexist or be readily achievable on LT4 standard therapy alone (Escobar-Morreale et al. 1995, McAninch et al. 2015, Werneck de Castro et al. 2015). If T4 would only always work, but it does not. And the reasons are apparent from regulatory principles, biochemical studies, experimental treatments and clinical outcome studies.
5. Salmela: The diagnostics of hypothyroidism in adults 2015
Central hypothyroidism is very rare, and a fresh estimate of its prevalence is 1 % .
Secondary hypothyroidism is much more difficult to diagnose and probably underestimated.
Echo imaging of the thyroid is usually not required in the diagnostics of hypothyroidism. It is only required, if the thyroid gland feels enlarged or containing nodules during palpation.
This suggests a step back 100 years in medicine. Thyroid imaging by ultrasound has been adopted as a routine by doctors. Detection of an altered pattern can raise early suspicion of autoimmune diseases, and hypervascularisation is a sign of hyperthyroidism, let alone the detection of smaller thyroid nodules.
Lists of tens of symptoms have been collected on certain Internet sites. These symptoms are said to point to hypothyroidism. These symptoms are non-specific, and they can be found in many other diseases as well. These symptoms are present especially in somatisation disorders and may be caused by major psychological trauma.
A careful history is key to diagnosis. Depressed people are frequently tired in the morning when they wake up, while many endocrine patients get tired over the course of the day. It is important to study and teach the art on how to ask the best questions.
The diagnosis of hypothyroidism isn't based on symptoms, because none of the symptoms and clinical signs is sensitive and specific enough. The diagnosis is based on laboratory findings.
The diagnostic process involves a combination and a probability chain. Sometimes we are made aware of the disease by a lab test and follow-up the test result, sometimes the patient presents with symptoms and we do the tests. But always is it a combination we consider.
According to clinical studies, the value of symptoms in the final diagnostics is less than 10 %.
Probably, the value of the doctor is low, if they do not assess symptoms very carefully.
Seriously, this can be readily dismissed scientifically according the Bayesian theorem, which appropriately deals with a combination of probabilities.
Those, who suffer from treatment resistant depression, may in up to 50 % of the cases be suffering from subclinical hypothyroidism. Still, the majority of depression patients have a normal thyroid function.
They may have a normal thyroid gland, but it is well known that depression affects thyroid function in many ways, as do many other diseases. See a pertinent recent review (Chatzitomaris et al. 2017).
Around 20 % of the endocrinologists measure T3 or FT3, but there are no good studies yet on the real clinical benefits of these measurements in the diagnostics of hypothyroidism. Especially the measurement of reduced concentrations, the immunological measurement methods used for FT3 in Finland might be problematic. This is why general practitioners should not use FT3 in the diagnostics of hypothyroidism. FT3 measurement is useful in the diagnostics of hyperthyroidism. rT3 should also not be used in general practice. It is also unclear, if the use of FT3 tests is useful in the follow up of T4 therapy.
Better standardisation of the methods is required so that the practitioner can rely on them. The manufacturers should be legally forced to harmonise their methods, so the assays agree on the true concentration. By law in many countries they need to measure precisely but not correctly. Using a scale analogy, 70 kg must be between say 69 and 71, but it could also be 49 to 51 or 89 to 91 with different methods. The major problem that still plagues all the thyroid assays in 2018 is insufficient harmonisation and calibration (Thienpont et al. 2010).
Elderly people often have only a few symptoms even in clinical hypothyroidism, whereas in some young individuals tiredness and mild cognitive impairment with diffculties in new learning and selective attention and concentration can already be observed in subclinical hypothyroidism. The symptoms of hypothyroidism are neither sensitive nor specifc and the diagnosis of hypothyroidism is based on S-TSH and S-fT4 concentrations. Many drugs and non-thyroidal illnesses can result in abnormal test results, and there are various analytical assay interferences such as human anti-animal antibodies in a patient’s serum, which can lead to falsely high S-TSH values. Subclinical hypothyroidism can progress to clinical hypothyroidism, especially in those with high positive values of serum TPO-ab and elevated S-TSH values.
The diagnostic process is a chain of various probabilities that are joined together and interpreted in their combination by the experienced doctor. The above description is alien to clinicians. We look at this from a reversed direction. A doctor starts with the patient, not the method and combines all the information available into a diagnostic assessment. The view from the disease is only helpful when we already know what it is but when we have to find out we have to reverse our view, like a good detective looking for all the evidence, and put it together.
Selected references
- Andersen S, Pedersen KM, Bruun NH, Laurberg P. Narrow individual variations in serum T(4) and T(3) in normal subjects: a clue to the understanding of subclinical thyroid disease. J Clin Endocrinol Metab (2002) 87:1068–1072. https://www.ncbi.nlm.nih.gov/pubmed/11889165
- Chatzitomaris A, Hoermann R, Midgley JE, Hering S, Urban A, Dietrich B, Abood A, Klein HH, Dietrich JW. Thyroid allostasis-adaptive responses of thyrotropic feedback control to conditions of strain, stress, and developmental programming. Front Endocrinol (2017) 8:163. doi:10.3389/fendo.2017.00163
- Escobar-Morreale HF, Obregón MJ, Escobar del Rey F, Morreale de Escobar G. Replacement therapy for hypothyroidism with thyroxine alone does not ensure euthyroidism in all tissues, as studied in thyroidectomized rats. J Clin Invest (1995) 96:2828–2838. doi:10.1172/JCI118353
- Gullo D, Latina A, Frasca F, Le Moli R, Pellegriti G, Vigneri R. Levothyroxine monotherapy cannot guarantee euthyroidism in all athyreotic patients. PLoS ONE (2011) 6:e22552. doi:10.1371/journal.pone.0022552
- Hoermann R, Eckl WA, Hoermann C, Larisch R. Complex relationship between free thyroxine and TSH in the regulation of thyroid function. Eur J Endocrinol (2010) 162:1123–1129. doi:10.1530/EJE-10-0106
- Hoermann R, Midgley JEM, Larisch R, Dietrich JW. Is pituitary TSH an adequate measure of thyroid hormone-controlled homoeostasis during thyroxine treatment? Eur J Endocrinol (2013) 168:271–280. doi:10.1530/EJE-12-0819
- Hoermann R, Midgley JEM, Giacobino A, Eckl WA, Wahl HG, Dietrich JW, Larisch R. Homeostatic equilibria between free thyroid hormones and pituitary thyrotropin are modulated by various influences including age, body mass index and treatment. Clin Endocrinol (Oxf) (2014) 81:907–915. doi:10.1111/cen.12527
- Hoermann R, Midgley JEM, Larisch R, Dietrich JW. Homeostatic control of the thyroid–pituitary axis: perspectives for diagnosis and treatment. Front Endocrinol (2015) 6:1–17. doi:10.3389/fendo.2015.00177
- Hoermann R, Larisch R, Dietrich JW, Midgley JEM. Derivation of a multivariate reference range for pituitary thyrotropin and thyroid hormones: diagnostic efficiency compared with conventional single-reference method. Eur J Endocrinol (2016) 174:735–743. doi:10.1530/EJE-16-0031
- Hoermann R, Midgley JEM, Larisch R, Dietrich JW. Relational stability in the expression of normality, variation, and control of thyroid function. Front Endocrinol (2016) 7:57–8. doi:10.3389/fendo.2016.00142
- Hoermann R, Midgley JEM, Larisch R, Dietrich JWC. Advances in applied homeostatic modelling of the relationship between thyrotropin and free thyroxine. PLoS ONE (2017) 12:e0187232–15. doi:10.1371/journal.pone.0187232
- Hoermann R, Midgley JEM, Dietrich JW, Larisch R. Dual control of pituitary thyroid stimulating hormone secretion by thyroxine and triiodothyronine in athyreotic patients. Ther Adv Endocrinol Metab (2017) 8:83–95. doi:10.1177/2042018817716401
- Hoermann R, Midgley JEM, Larisch R, Dietrich JW. Recent advances in thyroid hormone regulation: toward a new paradigm for optimal diagnosis and treatment. Front Endocrinol (2017) 8:57–8. doi:10.3389/fendo.2017.00364
- Ito M, Miyauchi A, Morita S, Kudo T, Nishihara E, Kihara M, Takamura Y, Ito Y, Kobayashi K, Miya A, et al. TSH-suppressive doses of levothyroxine are required to achieve preoperative native serum triiodothyronine levels in patients who have undergone total thyroidectomy. Eur J Endocrinol (2012) 167:373–378. doi:10.1530/EJE-11-1029
- Ito M, Miyauchi A, Hisakado M, Yoshioka W, Ide A, Kudo T, Nishihara E, Kihara M, Ito Y, Kobayashi K, et al. Biochemical markers reflecting thyroid function in athyreotic patients on levothyroxine monotherapy. Thyroid (2017) 27:484–490. doi:10.1089/thy.2016.0426
- Larisch R, Midgley JEM, Dietrich JW, Hoermann R. Symptomatic relief is related to serum free triiodothyronine concentrations during follow-up in levothyroxine-treated patients with differentiated thyroid cancer. Exp Clin Endocrinol Diabetes. 2018; doi: 10.1055/s-0043-125064.
- Leese GP, Soto-Pedre E, Donnelly LA. Liothyronine use in a 17 year observational population-based study - the TEARS study. Clin Endocrinol (Oxf) (2016) 85:918–925. doi:10.1111/cen.13052
- McAninch EA, Bianco AC. New insights into the variable effectiveness of levothyroxine monotherapy for hypothyroidism. Lancet Diab Endocrinol (2015) 3:756–758. doi:10.1016/S2213-8587(15)00325-3
- Midgley JEM, Larisch R, Dietrich JW, Hoermann R. Variation in the biochemical response to L-thyroxine therapy and relationship with peripheral thyroid hormone conversion. Endocr Connect (2015) 4:196-205. doi:10.1530/EC-15-0056
- Russell W, Harrison RF, Smith N, Darzy K, Shalet S, Weetman AP, Ross RJ. Free triiodothyronine has a distinct circadian rhythm that is delayed but parallels thyrotropin levels. J Clin Endocrinol Metab (2008) 93:2300–2306. doi:10.1210/jc.2007-2674
- Thienpont LM, Van Uytfanghe K, Beastall G, Faix JD, Ieiri T, Miller WG, Nelson JC, Ronin C, Ross HA, Thijssen JH, et al. Report of the IFCC Working Group for Standardization of Thyroid Function Tests; part 2: free thyroxine and free triiodothyronine. Clin Chem (2010) 56:912–920. doi:10.1373/clinchem.2009.140194
- Werneck de Castro JP, Fonseca TL, Ueta CB, McAninch EA, Abdalla SM, Wittmann G, Lechan RM, Gereben B, Bianco AC. Differences in hypothalamic type 2 deiodinase ubiquitination explain localized sensitivity to thyroxine. J Clin Invest (2015) 125:769–781. doi:10.1172/JCI77588
- Winther KH, Cramon P, Watt T, Bjorner JB, Ekholm O, Feldt-Rasmussen U, Groenvold M, Rasmussen ÅK, Hegedüs L, Bonnema SJ. Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS ONE (2016) 11:e0156925. doi:10.1371/journal.pone.0156925
Disclaimer
The brief responses provide general information only, adequate to encourage a scientific debate about the subject.
If more detailed information is sought the interested reader is referred to and encouraged to read the original scientific publications discussing the evidence.
However, this does not constitute medical advice nor is it meant to provide specific medical recommendations.
The views and opinions are my own and there is no conflict of interest to disclose.